
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Association of Measures of Glucose Metabolism with Colorectal Cancer Risk in Older Chinese: A 13-Year Follow-up of the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy and Meta-Analysis (Diabetes Metab J 2024;48:134-45)
- Shu Yi Wang, Lin Xu
- Diabetes Metab J. 2024;48(2):323-324. Published online March 22, 2024
- DOI: https://doi.org/10.4093/dmj.2024.0085
- 395 View
- 11 Download
- Metabolic Risk/Epidemiology
- Association of Measures of Glucose Metabolism with Colorectal Cancer Risk in Older Chinese: A 13-Year Follow-up of the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy and Meta-Analysis
- Shu Yi Wang, Wei Sen Zhang, Chao Qiang Jiang, Ya Li Jin, Tong Zhu, Feng Zhu, Lin Xu
- Diabetes Metab J. 2024;48(1):134-145. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0383

- 1,139 View
- 140 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Abnormal glucose metabolism is a risk factor for colorectal cancer (CRC). However, association of glycosylated hemoglobin (HbA1c) with CRC risk remains under-reported. We examined the association between glycemic indicators (HbA1c, fasting plasma glucose, fasting insulin, 2-hour glucose, 2-hour insulin, and homeostasis model of risk assessment-insulin resistance index) and CRC risk using prospective analysis and meta-analysis.
Methods
Participants (n=1,915) from the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy were included. CRC events were identified through record linkage. Cox regression was used to assess the associations of glycemic indicators with CRC risk. A meta-analysis was performed to investigate the association between HbA1c and CRC risk.
Results
During an average of 12.9 years follow-up (standard deviation, 2.8), 42 incident CRC cases occurred. After adjusting for potential confounders, the hazard ratio (95% confidence interval [CI]) of CRC for per % increment in HbA1c was 1.28 (95% CI, 1.01 to 1.63) in overall population, 1.51 (95% CI, 1.13 to 2.02) in women and 1.06 (95% CI, 0.68 to 1.68) in men. No significant association of other measures of glycemic indicators and baseline diabetes with CRC risk was found. Meta-analyses of 523,857 participants including our results showed that per % increment of HbA1c was associated with 13% higher risk of CRC, with the pooled risk ratio being 1.13 (95% CI, 1.01 to 1.27). Subgroupanalyses found stronger associations in women, colon cancer, Asians, and case-control studies.
Conclusion
Higher HbA1c was a significant predictor of CRC in the general population. Our findings shed light on the pathology of glucose metabolism and CRC, which warrants more in-depth investigation.
- Complications
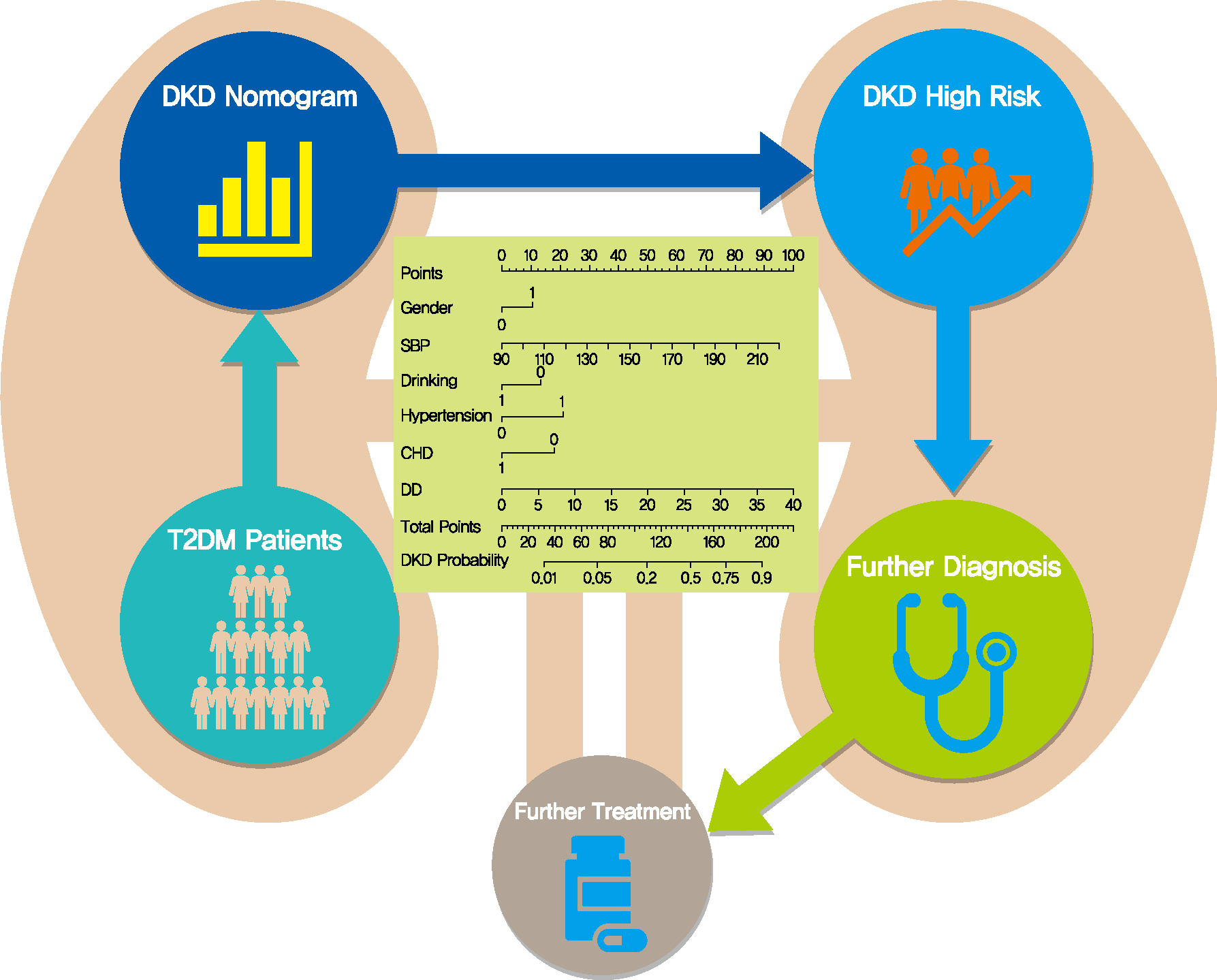
- Screening Tools Based on Nomogram for Diabetic Kidney Diseases in Chinese Type 2 Diabetes Mellitus Patients
- Ganyi Wang, Biyao Wang, Gaoxing Qiao, Hao Lou, Fei Xu, Zhan Chen, Shiwei Chen
- Diabetes Metab J. 2021;45(5):708-718. Published online April 13, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0117
- 6,927 View
- 141 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 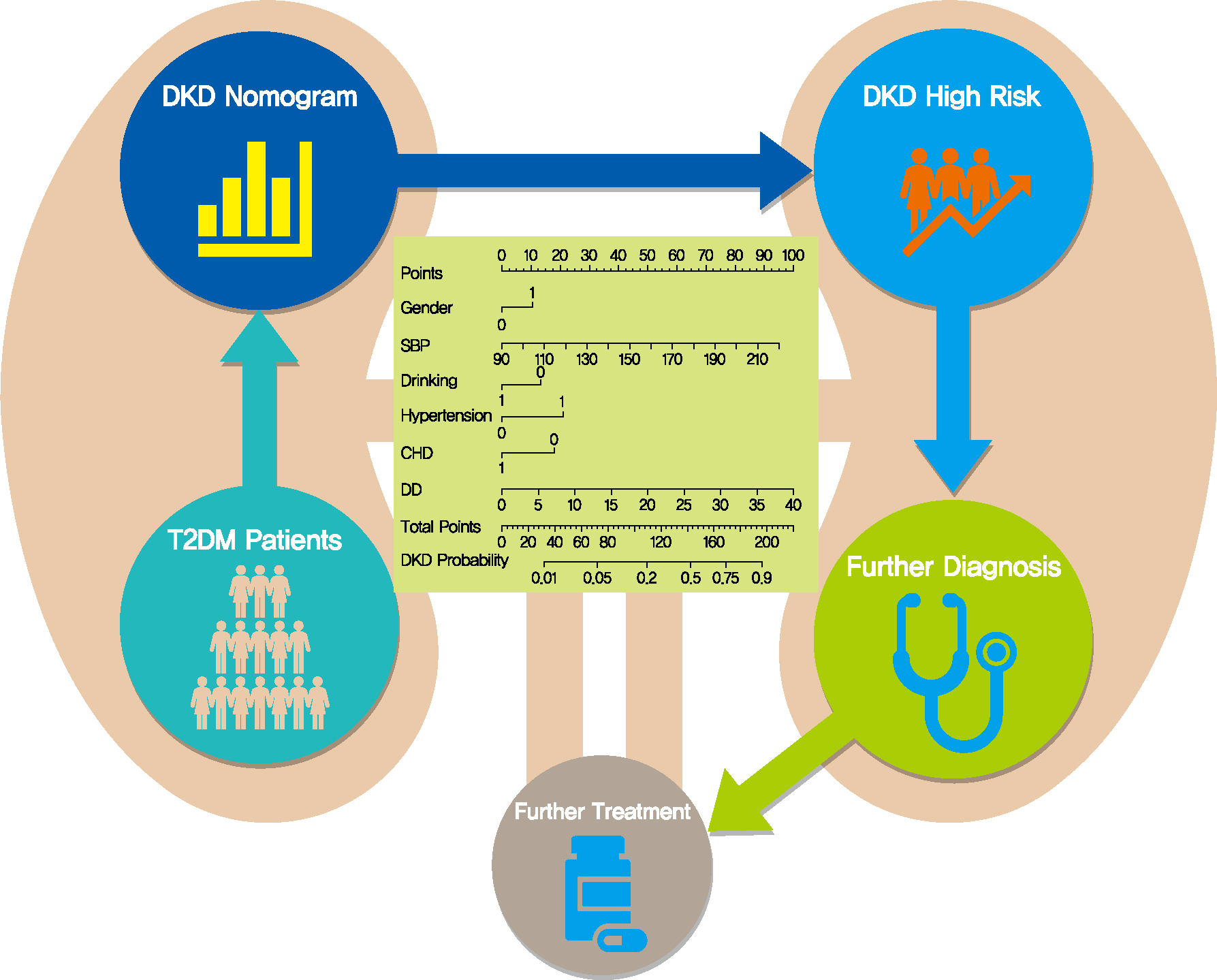
- Background
The influencing factors of diabetic kidney disease (DKD) in Chinese patients with type 2 diabetes mellitus (T2DM) were explored to develop and validate a DKD diagnostic tool based on nomogram approach for patients with T2DM.
Methods
A total of 2,163 in-hospital patients with diabetes diagnosed from March 2015 to March 2017 were enrolled. Specified logistic regression models were used to screen the factors and establish four different diagnostic tools based on nomogram according to the final included variables. Discrimination and calibration were used to assess the performance of screening tools.
Results
Among the 2,163 participants with diabetes (1,227 men and 949 women), 313 patients (194 men and 120 women) were diagnosed with DKD. Four different screening equations (full model, laboratory-based model 1 [LBM1], laboratory-based model 2 [LBM2], and simplified model) showed good discriminations and calibrations. The C-indexes were 0.8450 (95% confidence interval [CI], 0.8202 to 0.8690) for full model, 0.8149 (95% CI, 0.7892 to 0.8405) for LBM1, 0.8171 (95% CI, 0.7912 to 0.8430) for LBM2, and 0.8083 (95% CI, 0.7824 to 0.8342) for simplified model. According to Hosmer-Lemeshow goodness-of-fit test, good agreement between the predicted and observed DKD events in patients with diabetes was observed for full model (χ2=3.2756, P=0.9159), LBM1 (χ2=7.749, P=0.4584), LBM2 (χ2=10.023, P=0.2634), and simplified model (χ2=12.294, P=0.1387).
Conclusion
LBM1, LBM2, and simplified model exhibited excellent predictive performance and availability and could be recommended for screening DKD cases among Chinese patients with diabetes. -
Citations
Citations to this article as recorded by- Development of Serum Lactate Level-Based Nomograms for Predicting Diabetic Kidney Disease in Type 2 Diabetes Mellitus Patients
Chunxia Jiang, Xiumei Ma, Jiao Chen, Yan Zeng, Man Guo, Xiaozhen Tan, Yuping Wang, Peng Wang, Pijun Yan, Yi Lei, Yang Long, Betty Yuen Kwan Law, Yong Xu
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 1051. CrossRef - Changes in urinary exosomal protein CALM1 may serve as an early noninvasive biomarker for diagnosing diabetic kidney disease
Tao Li, Tian ci Liu, Na Liu, Man Zhang
Clinica Chimica Acta.2023; 547: 117466. CrossRef - Developing screening tools to estimate the risk of diabetic kidney disease in patients with type 2 diabetes mellitus
Xu Cao, Xiaomei Pei
Technology and Health Care.2023; : 1. CrossRef - Development and validation of a novel nomogram to predict diabetic kidney disease in patients with type 2 diabetic mellitus and proteinuric kidney disease
Hui Zhuan Tan, Jason Chon Jun Choo, Stephanie Fook-Chong, Yok Mooi Chin, Choong Meng Chan, Chieh Suai Tan, Keng Thye Woo, Jia Liang Kwek
International Urology and Nephrology.2022; 55(1): 191. CrossRef - Nomogram-Based Chronic Kidney Disease Prediction Model for Type 1 Diabetes Mellitus Patients Using Routine Pathological Data
Nakib Hayat Chowdhury, Mamun Bin Ibne Reaz, Sawal Hamid Md Ali, Shamim Ahmad, María Liz Crespo, Andrés Cicuttin, Fahmida Haque, Ahmad Ashrif A. Bakar, Mohammad Arif Sobhan Bhuiyan
Journal of Personalized Medicine.2022; 12(9): 1507. CrossRef - Development and assessment of diabetic nephropathy prediction model using hub genes identified by weighted correlation network analysis
Xuelian Zhang, Yao Wang, Zhaojun Yang, Xiaoping Chen, Jinping Zhang, Xin Wang, Xian Jin, Lili Wu, Xiaoyan Xing, Wenying Yang, Bo Zhang
Aging.2022; 14(19): 8095. CrossRef
- Development of Serum Lactate Level-Based Nomograms for Predicting Diabetic Kidney Disease in Type 2 Diabetes Mellitus Patients
- Complications
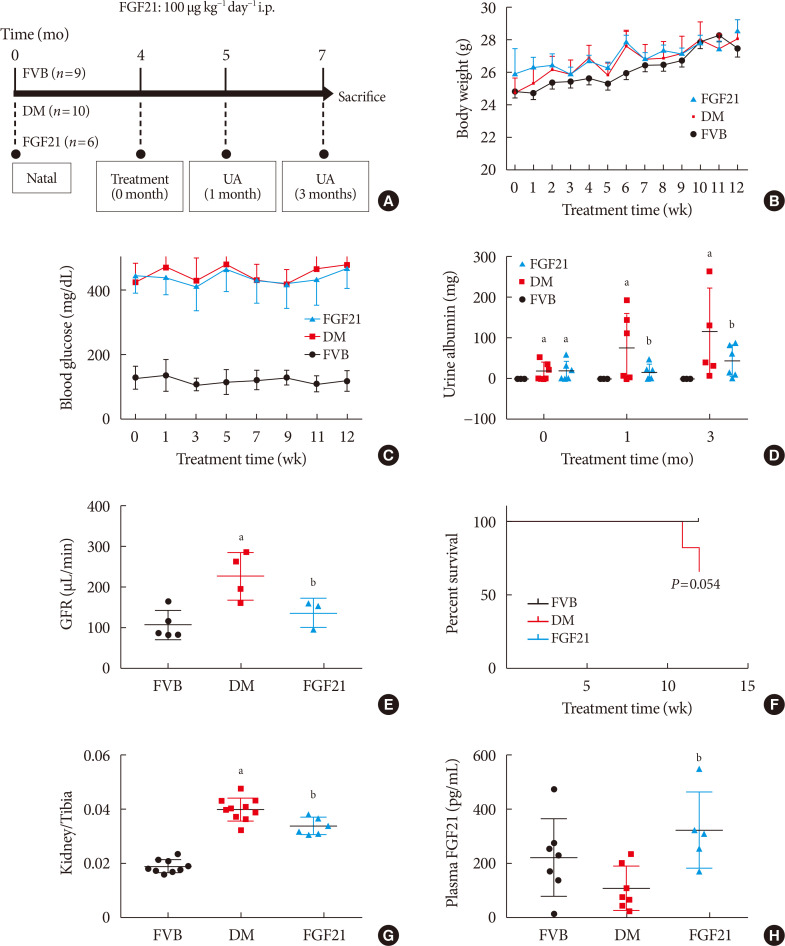
- Therapeutic Effects of Fibroblast Growth Factor-21 on Diabetic Nephropathy and the Possible Mechanism in Type 1 Diabetes Mellitus Mice
- Wenya Weng, Tingwen Ge, Yi Wang, Lulu He, Tinghao Liu, Wanning Wang, Zongyu Zheng, Lechu Yu, Chi Zhang, Xuemian Lu
- Diabetes Metab J. 2020;44(4):566-580. Published online May 15, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0089
- 5,919 View
- 102 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Fibroblast growth factor 21 (FGF21) has been only reported to prevent type 1 diabetic nephropathy (DN) in the streptozotocin-induced type 1 diabetes mellitus (T1DM) mouse model. However, the FVB (Cg)-Tg (Cryaa-Tag, Ins2-CALM1) 26OVE/PneJ (OVE26) transgenic mouse is a widely recommended mouse model to recapture the most important features of T1DM nephropathy that often occurs in diabetic patients. In addition, most previous studies focused on exploring the preventive effect of FGF21 on the development of DN. However, in clinic, development of therapeutic strategy has much more realistic value compared with preventive strategy since the onset time of DN is difficult to be accurately predicted. Therefore, in the present study OVE26 mice were used to investigate the potential therapeutic effects of FGF21 on DN.
Methods Four-month-old female OVE26 mice were intraperitoneally treated with recombinant FGF21 at a dose of 100 µg/kg/day for 3 months. The diabetic and non-diabetic control mice were treated with phosphate-buffered saline at the same volume. Renal functions, pathological changes, inflammation, apoptosis, oxidative stress and fibrosis were examined in mice of all groups.
Results The results showed that severe renal dysfunction, morphological changes, inflammation, apoptosis, and fibrosis were observed in OVE26 mice. However, all the renal abnormalities above in OVE26 mice were significantly attenuated by 3-month FGF21 treatment associated with improvement of renal adenosine 5′-monophosphate (AMP)-activated protein kinase (AMPK) activity and sirtuin 1 (SIRT1) expression.
Conclusion Therefore, this study demonstrated that FGF21 might exert therapeutic effects on DN through AMPK-SIRT1 pathway.
-
Citations
Citations to this article as recorded by- Fibroblast growth factor 21 alleviates unilateral ureteral obstruction-induced renal fibrosis by inhibiting Wnt/β-catenin signaling pathway
Wenhui Zhong, Yuheng Jiang, Huizhen Wang, Xiang Luo, Tao Zeng, Huimi Huang, Ling Xiao, Nan Jia, Aiqing Li
Biochimica et Biophysica Acta (BBA) - Molecular Cell Research.2024; 1871(2): 119620. CrossRef - Urinary Excretion of Biomolecules Related to Cell Cycle, Proliferation, and Autophagy in Subjects with Type 2 Diabetes and Chronic Kidney Disease
Anton I. Korbut, Vyacheslav V. Romanov, Vadim V. Klimontov
Biomedicines.2024; 12(3): 487. CrossRef - New developments in the biology of fibroblast growth factors
David M. Ornitz, Nobuyuki Itoh
WIREs Mechanisms of Disease.2022;[Epub] CrossRef - SIRT1–SIRT7 in Diabetic Kidney Disease: Biological Functions and Molecular Mechanisms
Wenxiu Qi, Cheng Hu, Daqing Zhao, Xiangyan Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Research Progress of Fibroblast Growth Factor 21 in Fibrotic Diseases
Min-Qi Jia, Cha-Xiang Guan, Jia-Hao Tao, Yong Zhou, Liang-Jun Yan
Oxidative Medicine and Cellular Longevity.2022; 2022: 1. CrossRef - Metabolic-associated fatty liver disease increases the risk of end-stage renal disease in patients with biopsy-confirmed diabetic nephropathy: a propensity-matched cohort study
Yutong Zou, Lijun Zhao, Junlin Zhang, Yiting Wang, Yucheng Wu, Honghong Ren, Tingli Wang, Yuancheng Zhao, Huan Xu, Lin Li, Nanwei Tong, Fang Liu
Acta Diabetologica.2022; 60(2): 225. CrossRef - FGF21 and Chronic Kidney Disease
João Victor Salgado, Miguel Angelo Goes, Natalino Salgado Filho
Metabolism.2021; 118: 154738. CrossRef - The Multiple Roles of Fibroblast Growth Factor in Diabetic Nephropathy
Junyu Deng, Ye Liu, Yiqiu Liu, Wei Li, Xuqiang Nie
Journal of Inflammation Research.2021; Volume 14: 5273. CrossRef - Therapeutic effect and mechanism of combined use of FGF21 and insulin on diabetic nephropathy
Fanrui Meng, Yukai Cao, Mir Hassan Khoso, Kai Kang, Guiping Ren, Wei Xiao, Deshan Li
Archives of Biochemistry and Biophysics.2021; 713: 109063. CrossRef - FGF19 and FGF21 for the Treatment of NASH—Two Sides of the Same Coin? Differential and Overlapping Effects of FGF19 and FGF21 From Mice to Human
Emma Henriksson, Birgitte Andersen
Frontiers in Endocrinology.2020;[Epub] CrossRef - FGF21: An Emerging Therapeutic Target for Non-Alcoholic Steatohepatitis and Related Metabolic Diseases
Erik J. Tillman, Tim Rolph
Frontiers in Endocrinology.2020;[Epub] CrossRef
- Fibroblast growth factor 21 alleviates unilateral ureteral obstruction-induced renal fibrosis by inhibiting Wnt/β-catenin signaling pathway
- Metabolic Risk/Epidemiology
- Association between Higher Blood Pressure and Risk of Diabetes Mellitus in Middle-Aged and Elderly Chinese Adults
- Xue Yang, Jian Chen, An Pan, Jason H.Y. Wu, Fei Zhao, Yue Xie, Yi Wang, Yi Ye, Xiong-Fei Pan, Chun-Xia Yang
- Diabetes Metab J. 2020;44(3):436-445. Published online November 14, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0081
- 4,831 View
- 83 Download
- 11 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To examine the prospective association between higher blood pressure (BP) and risk of type 2 diabetes mellitus (T2DM) in middle-aged and elderly Chinese adults.
Methods A total of 9,642 middle-aged and elderly Chinese adults (≥45 years old; 47.30% men) without diabetes from the China Health and Retirement Longitudinal Study were included for analyses. Participants were categorized into three groups: normal BP, prehypertension, and hypertension, according to the 2010 Chinese Guidelines for the Management of Hypertension. The incidence of T2DM was determined by self-reported physician diagnosis during two follow-up surveys conducted in 2013 to 2014 and 2015 to 2016.
Results During the 4-year follow-up, 429 participants (4.45%) developed T2DM, including 3.51% of the men and 5.29% of the women. The incidence rates of T2DM were 2.57%, 3.75%, and 6.71% in the normal BP, prehypertension, and hypertension groups, respectively. After adjustment for age, sex, education level, residence, smoking status, alcohol consumption, body mass index, waist circumference, and dyslipidemia, both prehypertension (odds ratio [OR], 1.32; 95% confidence interval [CI], 0.98 to 1.77) and hypertension (OR, 2.02; 95% CI, 1.54 to 2.64) were associated with increased risk of T2DM, compared to those with a normal BP. The ORs associated with T2DM were 1.08 (95% CI, 1.03 to 1.13) for an increase of 10 mm Hg in systolic BP and 1.06 (95% CI, 1.01 to 1.10) for an increase of 5 mm Hg in diastolic BP.
Conclusion Higher BP is a risk factor for T2DM in middle-aged and elderly Chines. It may be a potential target for diabetes prevention.
-
Citations
Citations to this article as recorded by- Leveraging IgG N-glycosylation to infer the causality between T2D and hypertension
Haotian Wang, Yuan Li, Weijie Cao, Jie Zhang, Mingyang Cao, Xiaoni Meng, Di Liu, Youxin Wang
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Externalizing traits: Shared causalities for COVID-19 and Alzheimer's dementia using Mendelian randomization analysis
Haotian Wang, Mingyang Cao, Yingjun Xi, Weijie Cao, Xiaoyu Zhang, Xiaoni Meng, Deqiang Zheng, Lijuan Wu, Wei Wang, Di Liu, Youxin Wang, Shibu Yooseph
PNAS Nexus.2023;[Epub] CrossRef - Causal Paradigm Between Common Comorbidities of Cardiovascular and Metabolism-Related Diseases in Elderly: Evidence from Cross-Sectional and Mendelian Randomization Studies
Junwang Gu, Qi Wang, Xuanhui Wu, Han Zhang, Chunmei Wu, Wei Qiu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2953. CrossRef - Hypertension, Arterial Stiffness, and Diabetes: a Prospective Cohort Study
Xue Tian, Yingting Zuo, Shuohua Chen, Yijun Zhang, Xiaoli Zhang, Qin Xu, Shouling Wu, Anxin Wang
Hypertension.2022; 79(7): 1487. CrossRef - Integrated analysis of probability of type 2 diabetes mellitus with polymorphisms and methylation of SLC30A8 gene: a nested case-control study
Fulan Hu, Yanyan Zhang, Pei Qin, Yang Zhao, Dechen Liu, Qionggui Zhou, Gang Tian, Quanman Li, Chunmei Guo, Xiaoyan Wu, Ranran Qie, Shengbing Huang, Minghui Han, Yang Li, Dongsheng Hu, Ming Zhang
Journal of Human Genetics.2022; 67(11): 651. CrossRef - Understanding Frailty: Probabilistic Causality between Components and Their Relationship with Death through a Bayesian Network and Evidence Propagation
Ricardo Ramírez-Aldana, Juan Carlos Gomez-Verjan, Carmen García-Peña, Luis Miguel Gutiérrez-Robledo, Lorena Parra-Rodríguez
Electronics.2022; 11(19): 3001. CrossRef - Novel lipid indicators and the risk of type 2 diabetes mellitus among Chinese hypertensive patients: findings from the Guangzhou Heart Study
Hai Deng, Peng Hu, Huoxing Li, Huanning Zhou, Xiuyi Wu, Maohua Yuan, Xueru Duan, Miaochan Lao, Chuchu Wu, Murui Zheng, Xiang Qian Lao, Wenjing Zhao, Xudong Liu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Trends and Comparisons of Blood Pressure and Fasting Plasma Glucose in Patients with Hypertension, Diabetes, and Comorbidity: 4-Year Follow-Up Data
Luxinyi Xu, Xiaotong Wen, Ying Yang, Dan Cui
Risk Management and Healthcare Policy.2022; Volume 15: 2221. CrossRef - Policyholder cluster divergence based differential premium in diabetes insurance
Benjiang Ma, Qing Tang, Yifang Qin, Muhammad Farhan Bashir
Managerial and Decision Economics.2021; 42(7): 1793. CrossRef - Association of hypertension and incident diabetes in Chinese adults: a retrospective cohort study using propensity-score matching
Yang Wu, Haofei Hu, Jinlin Cai, Runtian Chen, Xin Zuo, Heng Cheng, Dewen Yan
BMC Endocrine Disorders.2021;[Epub] CrossRef
- Leveraging IgG N-glycosylation to infer the causality between T2D and hypertension

 KDA
KDA
 First
First Prev
Prev





